Atherosclerosis
Atherosclerosis
When pipes get clogged, its usually because we flushed something down the drain we shouldn’t have. Sometimes, build-up inside of pipes causes clogging. In arteriosclerosis, the walls of the arteries become thick and stiff and hypertension results. In atherosclerosis, which is the most common form of arteriosclerosis, small patchy areas called atheromas form that can block the vessel lumen and cause arterial spasms.
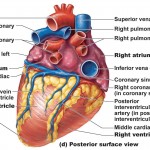
All arteries are susceptible to atherosclerosis, but the aorta, coronary and carotid arteries are affected most.
It’s been said that atherosclerosis indirectly causes half of the deaths in the modern world every year. How does this happen? The development of a atheroma or clot is said to occur in stages:
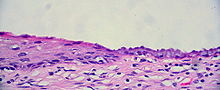
- The endothelium is injured — the initial stimulus is damage to the tunica intima caused by chemicals in the blood, components of cigarette smoke, hypertension, or bacterial or viral infections. Researchers suggest that almost any chronic infection can set the stage for atherosclerosis. Any injury to the endothelium sets of the alarm and the immune system responds causing an inflammatory response meant to repair the damage.
- Lipids accumulate and oxidize in the tunica intima — injured endothelial cells release chemotactic agents and growth factors and begin to transport and modify lipids picked up from blood, particularly low-density lipoproteins (LDL’s) that deliver cholesterol to tissue cells. The built-up LDL oxidizes in the inflammatory environment damaging the neighboring cells. It also acts as a chemotactic agent and attracts macrophages. Some of the macrophages become engorged with LDL’s and end up transforming into lipid-laden foam cells. Built-up foam cells form a fatty streak, the first visible sign of an atheroma.
- Smooth muscle cells proliferate and a fibrous cap forms — smooth muscle cells from the tunica media migrate and deposit elastic and collagen fibers thickening the intima and producing lesions with a core of dead and dying foam cells called atheroslerotic plaques. Initially, vessel walls will expand to accommodate the growing plaque, but eventually, the plaque will begin to block parts of the vessel lumen. At this point, the patient would be diagnosed with atherosclerosis.

- The plaque becomes unstable — As the plaque continues to grow, the cells in its center die. Then, calcium is deposited and collagen fiber production by smooth muscle cells declines. The plaque is now called complicated plaque and may rupture.
The presence of plaque stiffens artery walls and results in hypertension. Increased pressure stresses the built-up plaque causing it to become even more unstable. Plaques also constrict the vessel and cause the walls to ulcerate, a condition that causes blood backup and thrombus formation. Two other factors promote thrombus formation:
- Endothelial cells damaged by plaque release nitric oxide and prostacyclin — these chemical inhibit platelet formation and promote vasodilation, so if cells that release these chemicals are damaged, the internal environment of vessels becomes clot friendly.
- Lipoprotein — is an altered form of LDL found in certain people. It inhibits fibrinolysis, thereby increasing clot formations.
Plaques formation increases the risk of myocardial infarction (heart attack), aneurysms, and strokes. It can also be the cause of angina (chest pain). At least one-third of all heart attacks are caused by plaques too small to be seen on a normal angiogram, so the myth that massive plaque build-up has to occur to cause a problem is completely false. Sometimes, there simply are no symptoms.
Risk factors for atherosclerosis include age, sex (particularly male), family history, hypertension, smoking, obesity, diabetes, stress, high blood cholesterol, and a sedentary lifestyle. A growing body of evidence shows a link between internal inflammation and the formation and rupture of atheroslerotic plaques. C-reactive protein is a marker of systemic inflammation and is measured to predict the likelihood of a future heart attack or stroke.
Prevention and treatment of atherosclerosis
A lot of risk factors are under your own control. For instance, you can avoid cigarettes, eat healthy and exercise regularly, but sometimes, it’s simply not enough. In these cases, a pharmaceutical approach is warranted. Originally, everyone hoped cholesterol-lowering drugs would clean vessel walls of plaque, and although statins lower LDL, they do very little when it comes to decreasing plaque build-up. They do have other benefits though. For instance, they act as anti-inflammatories which helps stabilize the existing plaques so they don’t rupture.
These clots can, potentially, cause a heart attack or another type of heart disease. If you notice that you have an irregular heartbeat, you might want to consider using something like a defibrillator to try and put your heart back in a normal rhythm. These devices usually have a long battery life, however, they can run out. In the event that your device battery runs out, you need to pick the right battery for your defibrillator. Be sure to seek expert advice if you’re unsure. Having a device like this will ensure that you have a better chance of saving yourself and your family if they ever experience any irregular heart problems. The American Heart Association recommended that people with higher chances of heart problems take one aspirin a day to prevent clot formation if clots do rupture. Perhaps having a defibrillator on hand is a good idea, just in case.
Larger plaques that block parts of arteries are treated in almost the same way we would treat a sewer pipe. In coronary bypass surgery, veins removed from the legs or small arteries removed from the thoracic cavity are implanted in the heart to restore myocardial (heart) circulation. In balloon angioplasty, a catheter with a balloon tightly packed into the tip is threaded through the vessels. When the catheter reaches the plaque, the balloon is inflated to compress the fatty mass against the vessel wall.
Angioplasty temporary clears the path but new blockages often occur. Stents, short small metal-mesh tubes, are inserted into the newly dilated vessels in order to hold the vessel open. Some stents release drugs that inhibit smooth muscle proliferation and help reduce new blockage, but they can become clogged over time as well.
When it comes to atherosclerosis, prevention is the best treatment. By making a few healthy lifestyle decisions, arteriosclerosis can be prevented and in some cases, completely avoided.
We hope you enjoyed the article and if you have any questions, feel free to leave a comment.
Related Posts
Category: Cardiovascular